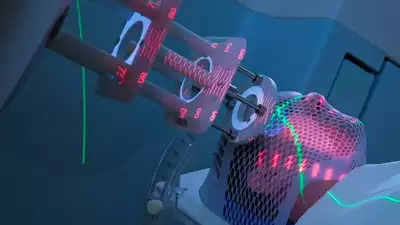
Discover how Flash radiotherapy is revolutionizing cancer treatment by delivering ultra-fast radiation, reducing side effects, and improving cure rates.
What is Flash Radiotherapy?
Flash radiotherapy is an innovative cancer treatment method that delivers ultra-high doses of radiation in less than a second. Unlike conventional radiotherapy, which requires multiple sessions and often damages healthy tissues, Flash radiotherapy significantly reduces treatment time and minimizes side effects.
This revolutionary technology uses radiation dose rates over 300 times higher than traditional methods. This speed induces the “FLASH effect,” which spares normal tissues while effectively targeting cancer cells.
How Does Flash Radiotherapy Work?
Traditional radiotherapy typically requires weeks of sessions, targeting tumors with incremental doses of radiation. However, Flash radiotherapy compresses this process into a single or limited number of sessions. It delivers:
- Ultra-fast radiation doses to eliminate cancer cells.
- Protection for surrounding healthy tissues, especially in sensitive areas like the brain.
The key lies in the high dose rate, which prevents damage to normal cells while maintaining its efficacy against tumors.

Proven Results in Animal and Human Trials
Preclinical animal studies have demonstrated the safety and efficacy of Flash radiotherapy. Building on these successes, a first-in-human trial conducted with metastatic cancer patients revealed promising outcomes:
- Patients experienced effective pain relief.
- No unexpected side effects were reported.
Dr. Emily C. Daugherty, lead author of the study and an assistant professor at the University of Cincinnati Cancer Center, highlighted its potential:
“Our study shows FLASH radiotherapy with protons is a practical modality to reduce pain. It deserves further exploration because of its potential to decrease the side effects associated with conventional treatments.”
Potential Benefits of Flash Radiotherapy
- Shortened Treatment Time
Patients may undergo treatment in a single session or significantly fewer sessions compared to conventional therapy. - Minimized Side Effects
According to Dr. John Breneman, a principal investigator in the trial:”FLASH radiotherapy causes less normal tissue injury, enabling larger doses of radiation to be delivered safely.” - Higher Cure Rates for Resistant Tumors
The ability to deliver larger radiation doses without increasing side effects offers hope for patients with tumors that are resistant to traditional treatments.
Challenges in Accessibility
Despite its potential, the widespread adoption of Flash radiotherapy faces significant hurdles:
- Advanced Equipment Requirements:
Current radiotherapy machines lack the capability to deliver the ultra-high dose rates necessary for Flash treatment. - Technological Innovations Needed:
Experts emphasize the need for advancements in generating FLASH photons, protons, and heavy ions to make this treatment accessible to a broader population.
A 2022 study underscores this challenge:
“Major technological advances are needed to enable the generation of FLASH photons, and potentially of protons, VHEE, and heavy ions.”
The Future of Cancer Treatment with Flash Radiotherapy
Flash radiotherapy represents a paradigm shift in oncology. With its ability to deliver rapid, effective treatment while reducing side effects, it holds immense promise for cancer patients worldwide.
However, for this technology to become mainstream, investments in research and development are critical. Once the accessibility challenges are addressed, Flash radiotherapy could:
- Revolutionize cancer care.
- Increase survival rates for resistant tumors.
- Reduce the burden of long-term side effects for patients.
Conclusion
Flash radiotherapy is an exciting advancement in cancer treatment, offering the potential to cure cancer in record time while safeguarding healthy tissues. As technological barriers are overcome, this groundbreaking therapy could become the standard of care for millions battling cancer worldwide.
Keywords: